Abstract
INTRODUCTION: Iron supplementation in iron deficiency anemia is standard practice, but the benefits of iron supplementation in iron deficient non-anemic (IDNA) individuals remains controversial. We conducted a systematic review and meta-analysis to identify the effects of iron therapy on fatigue and work capacity in iron deficient non-anemic adults.
METHODS: We included randomized controlled trials of adults (≥18 years) who were iron deficient but non-anemic. Interventions included oral, intramuscular or intravenous iron supplementation; all therapy doses, frequencies and durations were included. We included trials that evaluated outcomes at least 1 month from the initiation of iron therapy. Comparators included placebo or active therapy. Our primary outcome measures were self-reported fatigue and objective measures of work capacity. Secondary outcomes included the incidence of anemia, change in hemoglobin concentration and serum ferritin, and the incidence of adverse outcomes including iron toxicity, constipation, diarrhea, gastrointestinal intolerance and nausea. We searched Medline, Embase, CENTRAL, CINAHL, SportDiscus, and CAB Abstracts from inception to October 31, 2016. We searched the World Health Organization's ICTRP for relevant ongoing trials and performed forward searches of included trials and relevant reviews in Web of Science. We assessed internal validity of included trials using the Cochrane Risk of Bias tool, and the external validity using the GRADE methodology.
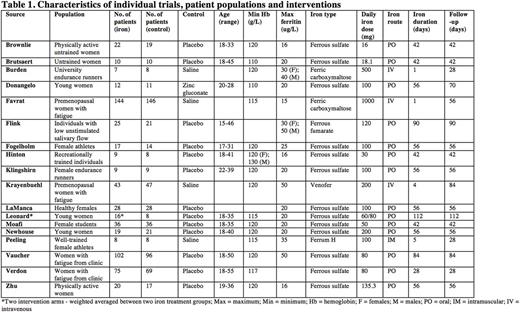
RESULTS: From 11580 citations we included 18 unique trials, and 2 companion papers enrolling 1162 patients (Table 1). Trials were published between 1989 and 2015, and all trials were published in peer-reviewed journals. Exclusively healthy females (aged 17 to 55 years old) with varying levels of fitness (sedentary to well-trained) were enrolled in all but three studies. Iron interventions consisted of iron supplementation administered orally, intramuscularly or intravenously. Of the trials evaluating oral supplements, all but one used ferrous sulfate (13 trials, 721 participants). Intravenous iron was administered in three trials (395 participants), and intramuscular iron in one trial (16 participants). In trials using oral iron, the mean daily elemental iron dose was 86.9mg (± 49.1mg; range: 16 to 200mg). In trials reporting intravenous iron, the mean daily elemental iron dose was 566mg (± 330mg; range 200 to 1000mg) and mean total elemental iron dose 767mg (± 206mg; range 500 to 1000mg). Among all studies, the mean duration of iron therapy was 46 days (± 30 days; range 1 to 112 days), and mean duration of follow-up was 57 days (± 24 days; range 28 to 112 days). Fatigue was evaluated in four trials enrolling 714 participants. Iron supplementation was associated with a reduction in subjective measures of fatigue when assessed by either the Piper Fatigue Scale (PFS), the Current and Past Psychological State scale (CAPPS), visual analog scale or Brief Fatigue Inventory questionnaire (BFI) (SMD -0.38; 95% CI -0.52 to -0.23; I2 0%). Work capacity was reported in 10 trials (291 participants); all but one of the trials employed at least one of three common aerobic tests of work capacity: time trial, time to exhaustion, or VO2 max performance from a graded exercise test. In two trials (79 participants) that used 15 km time trials, iron supplementation was not associated with improved exercise capacity (SMD -0.09; 95% CI -0.53 to 0.35; I2 0%). In four trials (69 participants) that used time-to-exhaustion tests, iron supplementation did not significantly improve exercise capacity (SMD 0.25; 95% CI -0.22 to 0.73; I2 0%). Nine trials (235 participants) reported VO2 max as a surrogate measure of work capacity. Iron supplementation did not increase VO2 max (SMD 0.11; 95% CI -0.15 to 0.37; I2 0%).
CONCLUSION: In iron deficient non-anemic adults, iron supplementation is associated with reduced subjective measures of fatigue, but not with objective improvements in work capacity. Given the global prevalence of both iron deficiency and fatigue, patients and practitioners could consider a course of iron supplementation to improve symptoms of fatigue in presence or absence of documented anemia.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal